Ocular melanoma
What is ocular melanoma?
Ocular melanoma is a rare cancer that begins in the melanocytes (pigment-producing cells) of the eye. Just like skin melanoma, it develops from the cells that give colour to our eyes and skin, but it forms in different parts of the eye.
Though it is rare, ocular melanoma is the most common type of eye cancer in adults. It behaves differently from skin melanoma and requires specialised care.
Types of ocular melanoma
Ocular melanoma can occur in different parts of the eye.
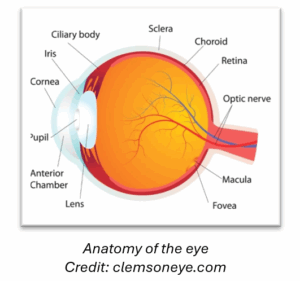
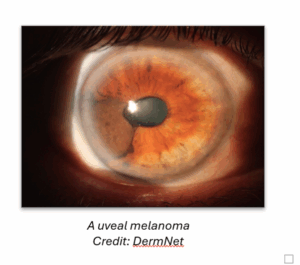
- Uveal melanoma (the most common form) occurs in the uvea, which includes the iris (coloured part of the eye), ciliary body (involved in producing fluid), and choroid (the layer behind the retina).
- Conjunctival melanoma occurs on the surface of the eye, often starting as a pigmented spot.
- Orbital or eyelid melanoma (very rare) begins in the skin around the eye or within the orbit (eye socket).
Risk factors for ocular melanoma
Ocular melanoma may not cause symptoms in its early stages, but it may be picked up during routine eye checks. Symptoms may include:
- blurred or distorted vision
- a dark spot on the iris
- flashing lights or floaters
- a change in the shape of the pupil
- loss of the visual field
- a red or irritated eye (rarely).
If you experience any of these symptoms you should discuss them with an ophthalmologist (eye specialist) promptly.
Preventing ocular melanoma by protecting your eyes from UV damage
Although the exact causes of ocular melanoma are still being studied, and some risk factors like eye colour and family history are beyond your control, reducing UV exposure to the eyes is a practical way to help lower your risk.
- Wear sunglasses that block 99 to 100% of both UVA and UVB rays. This helps protect the delicate tissues inside your eyes.
- Use a wide-brimmed hat to reduce UV exposure to your eyes and face.
- Apply sunscreen safely. When you are not wearing sunglasses, use a broad-spectrum at least SPF 30 sunscreen suitable for the face and around the eyes.
- Don’t be fooled by clouds. UV rays can still damage your eyes on overcast days.
- Take care near reflective surfaces. Water, sand, snow and concrete can reflect UV rays.
How to detect ocular melanoma early
Early detection gives the best chance of effective treatment.
- Have regular eye exams with an ophthalmologist or optometrist. These are important even if you don’t have symptoms.
- Speak up about changes. If you notice blurred vision, flashing lights, floaters, or any new visual symptoms, see your eye specialist as soon as possible.
Diagnosing ocular melanoma
Ocular melanoma is usually diagnosed by an ophthalmologist using:
- an eye examination with dilated pupils
- an ultrasound scan of the eye
- ocular coherence tomography (OCT)
- angiography (special imaging of blood vessels)
- an MRI or CT scan (to check for spread).
A biopsy is not always needed as ocular melanoma often has characteristic imaging features.
Treatment options
Treatment depends on the type, size and location of the tumour, and whether it has spread. It is usually coordinated by a specialist ocular oncology team.
Treatments for localised melanoma include:
- radiation therapy (commonly plaque brachytherapy or proton beam therapy)
- surgical removal of the tumour or the eye (enucleation) in some cases
- laser treatment (less commonly used).
Treatments for advanced/metastatic melanoma include:
- systemic therapies like immunotherapy or targeted therapy (in clinical trials or specialist centres)
- palliative care to manage symptoms and improve quality of life.
Prognosis
Prognosis varies depending on the tumour’s location, size and genetic changes, and whether the melanoma has spread.
- Many small, localised ocular melanomas are treatable and have good outcomes.
- Uveal melanoma has a risk of spreading (particularly to the liver), even years after treatment.
Regular follow-up and monitoring are essential.
Follow-up care
You are likely to need ongoing care involving:
- regular eye checks and imaging
- monitoring for metastasis (commonly with liver ultrasounds or MRIs)
- supportive care for vision or psychological wellbeing.
Your care team may include an ophthalmologist, oncologist, specialises nurse, GP, and support organisations.
Living with ocular melanoma
Being diagnosed with ocular melanoma can be overwhelming. You may experience changes in your vision, body image or emotional wellbeing. Support is available:
- Talk to your healthcare team about counselling or peer support
- Inform your GP and have regular health checks
- Connect with Melanoma New Zealand for its support services and networks
- Connect with this Facebook Ocular Melanoma Support Group: OcuMel Australia and New Zealand (Ocular Melanoma Support) | Facebook
Questions to ask your specialist
- What type of ocular melanoma do I have?
- Has the melanoma spread?
- What are my treatment options?
- Will I lose vision in the affected eye?
- How will this affect my daily life?
- Are clinical trials available to me?
- What support services can I access?
Remember
- Ocular melanoma is rare and different from skin melanoma
- Early detection and specialised care are key.
- Support is available – you’re not alone
